Time slot's time in Taipei (GMT+8)
2025/11/21 08:30-13:00 Room 201 DEF
- Kick-on Seminar IV
Intraoperative Neurophysiologic Monitoring (IONM): The Current Status We Are and Future Targets We Approach
- Time
- Topic
- Speaker
- Moderator
- 08:30-09:00
- An overview of intraoperative neurophysiology monitoring: the advances and challenges
- Speaker:
Tsui-Fen Yang
- Moderator:
Huai-Che Yang
- Tsui-Fen Yang
- MD
-
Affiliated attending physician, Department of physical medicine and rehabilitation, Taipei Veterans General Hospital
E-mail:tsuifenyang1@gmail.com
Executive Summary:
Dr. Tsui-Fen Yang graduated from National Yang-Ming University and completed her residency training in Physical Medicine and Rehabilitation at Taipei Veterans General Hospital. She previously served as the Director of the Neurorehabilitation Division and is currently an attending physician affiliated with both the Department of Physical Medicine and Rehabilitation at Taipei Veterans General Hospital and the Department of Rehabilitation Medicine at Changhua Christian Hospital.
Dr. Yang specializes in pediatric rehabilitation, neurorehabilitation, dysphagia management, scoliosis, and intraoperative neurophysiological monitoring (IONM). With over 17 years of experience in the field, she has published several relevant articles and is highly experienced in intraoperative monitoring, dedicating approximately one-third of her clinical time to monitoring pediatric patients. She also plays a key role in training new professionals in IONM in Taiwan through an annual national training program.
Dr. Tsui-Fen Yang graduated from National Yang-Ming University and completed her residency training in Physical Medicine and Rehabilitation at Taipei Veterans General Hospital. She previously served as the Director of the Neurorehabilitation Division and is currently an attending physician affiliated with both the Department of Physical Medicine and Rehabilitation at Taipei Veterans General Hospital and the Department of Rehabilitation Medicine at Changhua Christian Hospital.
Dr. Yang specializes in pediatric rehabilitation, neurorehabilitation, dysphagia management, scoliosis, and intraoperative neurophysiological monitoring (IONM). With over 17 years of experience in the field, she has published several relevant articles and is highly experienced in intraoperative monitoring, dedicating approximately one-third of her clinical time to monitoring pediatric patients. She also plays a key role in training new professionals in IONM in Taiwan through an annual national training program.
Lecture Abstract:
An overview of intraoperative neurophysiology monitoring: the advances and challenges
Tsui-Fen Yang, MD
Affiliated Attending Physician at Department of Physical Medicine & Rehabilitation, Taipei Veterans General Hospital, and Changhua Christian Hospital, Taiwan
In certain neurosurgical and orthopedic procedures, while achieving the intended therapeutic goals, there is a risk of injury to certain nerves. Over the past few decades, intraoperative neurophysiological monitoring (IONM) techniques have been rapidly evolving to meet the demands of such surgeries. Different types of surgeries pose risks to different neural structures; therefore, monitoring strategies are tailored accordingly.
Currently, there are various monitoring modalities available, including Motor Evoked Potentials (MEP), Somatosensory Evoked Potentials (SSEP), Electromyography (EMG), Visual Evoked Potentials (VEP), Brainstem Auditory Evoked Potentials (BAEP), electroencephalography (EEG), and even regional reflexes. These can be selectively combined in what is referred to as a multimodality approach, with the goal of achieving both surgical success and functional preservation. Excitingly, intraoperative monitoring techniques continue to advance, aiming to further enhance surgical safety.
However, the implementation of IONM does come with challenges. For example, preexisting neurological deficits or varying degrees of paralysis can affect monitoring. Additionally, very young or elderly patients present technical difficulties. Underlying medical conditions may also interfere with monitoring. Moreover, anesthetic agents can impact signal quality, and maintaining stable intraoperative hemodynamics is another critical consideration.
In recent years, there has been an increasing emphasis on evidence-based practice in all medical procedures. However, one of the practical challenges with IONM is that its effectiveness cannot easily be validated through randomized controlled trials (RCTs). Furthermore, for relatively simple procedures, whether IONM is necessary raises questions of cost-effectiveness. This presentation aims to address these issues and provide an overview of the current state and considerations surrounding intraoperative monitoring.
An overview of intraoperative neurophysiology monitoring: the advances and challenges
Tsui-Fen Yang, MD
Affiliated Attending Physician at Department of Physical Medicine & Rehabilitation, Taipei Veterans General Hospital, and Changhua Christian Hospital, Taiwan
In certain neurosurgical and orthopedic procedures, while achieving the intended therapeutic goals, there is a risk of injury to certain nerves. Over the past few decades, intraoperative neurophysiological monitoring (IONM) techniques have been rapidly evolving to meet the demands of such surgeries. Different types of surgeries pose risks to different neural structures; therefore, monitoring strategies are tailored accordingly.
Currently, there are various monitoring modalities available, including Motor Evoked Potentials (MEP), Somatosensory Evoked Potentials (SSEP), Electromyography (EMG), Visual Evoked Potentials (VEP), Brainstem Auditory Evoked Potentials (BAEP), electroencephalography (EEG), and even regional reflexes. These can be selectively combined in what is referred to as a multimodality approach, with the goal of achieving both surgical success and functional preservation. Excitingly, intraoperative monitoring techniques continue to advance, aiming to further enhance surgical safety.
However, the implementation of IONM does come with challenges. For example, preexisting neurological deficits or varying degrees of paralysis can affect monitoring. Additionally, very young or elderly patients present technical difficulties. Underlying medical conditions may also interfere with monitoring. Moreover, anesthetic agents can impact signal quality, and maintaining stable intraoperative hemodynamics is another critical consideration.
In recent years, there has been an increasing emphasis on evidence-based practice in all medical procedures. However, one of the practical challenges with IONM is that its effectiveness cannot easily be validated through randomized controlled trials (RCTs). Furthermore, for relatively simple procedures, whether IONM is necessary raises questions of cost-effectiveness. This presentation aims to address these issues and provide an overview of the current state and considerations surrounding intraoperative monitoring.
- Time
- Topic
- Speaker
- Moderator
- 09:00-09:30
- New insights on intraoperative motor evoked potential monitoring in cervical myelopathy?
- Speaker:
Yew Long Lo
- Moderator:
Tsui-Fen Yang
- Yew Long Lo
- MD
-
Senior Consultant Neurologist, National Neuroscience Institute, Singapore General Hospital
E-mail:lo.yew.long@singhealth.com.sg
Executive Summary:
Professor Lo graduated from the National University of Singapore and joined the Department of Neurology, Singapore General Hospital in 1994. He completed his postgraduate fellowship in Clinical Neurophysiology at the University of Oxford in 1998. He has been a fellow of the Academy of Medicine, Singapore, since 1999. He was previously Head and currently Deputy Chief Executive Officer and Senior Consultant Neurologist at the National Neuroscience Institute (SGH Campus) and Professor, Duke-NUS Medical School, Adjunct Professor, Lee Kong Chian School of Medicine and Adjunct Professor, Faculty of Medicine, National University of Singapore. Prof Lo served as the Chairman of the Centralised Institutional Review Board, and is currently Group Director of Research Integrity, Compliance and Ethics at SingHealth.
Professor Lo is active in the field of Clinical Neurophysiology and lectures regularly on this subject in the USA, Europe, Australasia and Asian countries. . He was the founder president of the Clinical Neurophysiology Society (Singapore) and representative to the International Federation of Clinical Neurophysiology. He was an invited speaker in the World and Asian Oceanian Congresses of Neurology, as well as the European and International Congress of Clinical Neurophysiology. He is the current President of the Asian-Oceanian Society of Intraoperative Neurophysiology (AOSIN). In 2007, he was the awarded the Galloway Lectureship for his work in cervical myelopathy. He delivered the 31st Seah Cheng Siang Memorial Lecture in 2022 on intraoperative monitoring of surgical procedures. He received the Public Administration Medal at the National Day Awards in 2024.
His main research interests are on spinal cord disorders, where he has held 3 National Medical Research Grants. He is principal investigator of projects addressing the functional neurophysiology of cord compression, mechanisms of cervical whiplash and cortical plasticity changes in spinal cord dysfunction. Other ongoing international research collaborations include transcranial magnetic stimulation in motor control, neuromuscular transmission in demyelinating neuropathies and imaging correlates of cortical and cerebellar activity.
Professor Lo is Associate Editor of Clinical Neurophysiology journal, serves on the current editorial board of Clinical Neurology and Neurosurgery and is a regular reviewer of over 30 international journals. He is past Editor-in-Chief of the Proceedings of Singapore Healthcare. He has over 200 publications in international peer reviewed journals, including first author papers in the New England Journal of Medicine, Neurology, The Lancet Neurology, Annals of Neurology, Brain, JAMA Neurology, Journal of Neurology, Spine, Journal of Neurology, Neurosurgery and Psychiatry, Nature Clinical Reviews Neurology, Journal of Medical Virology and Movement Disorders.
His book titled “Clinical Neurophysiology: New Clinical and Research Applications” is published in 2013.
Professor Lo graduated from the National University of Singapore and joined the Department of Neurology, Singapore General Hospital in 1994. He completed his postgraduate fellowship in Clinical Neurophysiology at the University of Oxford in 1998. He has been a fellow of the Academy of Medicine, Singapore, since 1999. He was previously Head and currently Deputy Chief Executive Officer and Senior Consultant Neurologist at the National Neuroscience Institute (SGH Campus) and Professor, Duke-NUS Medical School, Adjunct Professor, Lee Kong Chian School of Medicine and Adjunct Professor, Faculty of Medicine, National University of Singapore. Prof Lo served as the Chairman of the Centralised Institutional Review Board, and is currently Group Director of Research Integrity, Compliance and Ethics at SingHealth.
Professor Lo is active in the field of Clinical Neurophysiology and lectures regularly on this subject in the USA, Europe, Australasia and Asian countries. . He was the founder president of the Clinical Neurophysiology Society (Singapore) and representative to the International Federation of Clinical Neurophysiology. He was an invited speaker in the World and Asian Oceanian Congresses of Neurology, as well as the European and International Congress of Clinical Neurophysiology. He is the current President of the Asian-Oceanian Society of Intraoperative Neurophysiology (AOSIN). In 2007, he was the awarded the Galloway Lectureship for his work in cervical myelopathy. He delivered the 31st Seah Cheng Siang Memorial Lecture in 2022 on intraoperative monitoring of surgical procedures. He received the Public Administration Medal at the National Day Awards in 2024.
His main research interests are on spinal cord disorders, where he has held 3 National Medical Research Grants. He is principal investigator of projects addressing the functional neurophysiology of cord compression, mechanisms of cervical whiplash and cortical plasticity changes in spinal cord dysfunction. Other ongoing international research collaborations include transcranial magnetic stimulation in motor control, neuromuscular transmission in demyelinating neuropathies and imaging correlates of cortical and cerebellar activity.
Professor Lo is Associate Editor of Clinical Neurophysiology journal, serves on the current editorial board of Clinical Neurology and Neurosurgery and is a regular reviewer of over 30 international journals. He is past Editor-in-Chief of the Proceedings of Singapore Healthcare. He has over 200 publications in international peer reviewed journals, including first author papers in the New England Journal of Medicine, Neurology, The Lancet Neurology, Annals of Neurology, Brain, JAMA Neurology, Journal of Neurology, Spine, Journal of Neurology, Neurosurgery and Psychiatry, Nature Clinical Reviews Neurology, Journal of Medical Virology and Movement Disorders.
His book titled “Clinical Neurophysiology: New Clinical and Research Applications” is published in 2013.
Lecture Abstract:
Motor evoked potentials (MEP) are crucial for intraoperative monitoring (IOM) of spinal surgery. In decompressive surgery for cervical spondylotic myelopathy (CSM), recording of MEP is challenging as responses may be low in amplitude, inconsistent or even not elicitable. Other confounders could include, but not limited to, cortical excitability threshold, bony skull characteristics, metabolism of anaesthetic agents and severity of CSM.
Several developments have been made to facilitate MEP recordings, including use of longer cortical stimulation train pulses and double trains.
Many updated IOM cortical stimulators can deliver up to 9 pulses per train. It was found in a cohort of 20 patients with various spinal cord disorders that a shorter conditioning train of 2 pulses followed by a testing train of 7 pulses most effectively elicited MEPs in the lower limbs (Kale et al, 2020).
However, in 40 patients with severe CSM, we found that MEP amplitudes obtained were not different using 5, 7, 9 or 2 (conditioning)+ 7 (test) or 4 (conditioning) +5 (test) pulses in the upper and lower limbs. The only exception is for the upper limbs, when MEP amplitudes were lower when comparing 5 pulse stimulation with the other 4 conditions.
MEP latencies were significantly longer for both 2 + 7 and 4 + 5 pulse stimulations compared with either 5, 7 and 9 pulse stimulation bilaterally. This was observed in the upper and lower limb recordings.
CSM is known to result in cortical reorganization both before and after decompression surgery (Green t al, 2015). Our findings suggest that the temporal priming effects of double train stimulation may be negated in severe CSM at the cortical or spinal levels. Thus, the use of differential cortical stimulating positions should be explored as a spatial modifying strategy.
Motor evoked potentials (MEP) are crucial for intraoperative monitoring (IOM) of spinal surgery. In decompressive surgery for cervical spondylotic myelopathy (CSM), recording of MEP is challenging as responses may be low in amplitude, inconsistent or even not elicitable. Other confounders could include, but not limited to, cortical excitability threshold, bony skull characteristics, metabolism of anaesthetic agents and severity of CSM.
Several developments have been made to facilitate MEP recordings, including use of longer cortical stimulation train pulses and double trains.
Many updated IOM cortical stimulators can deliver up to 9 pulses per train. It was found in a cohort of 20 patients with various spinal cord disorders that a shorter conditioning train of 2 pulses followed by a testing train of 7 pulses most effectively elicited MEPs in the lower limbs (Kale et al, 2020).
However, in 40 patients with severe CSM, we found that MEP amplitudes obtained were not different using 5, 7, 9 or 2 (conditioning)+ 7 (test) or 4 (conditioning) +5 (test) pulses in the upper and lower limbs. The only exception is for the upper limbs, when MEP amplitudes were lower when comparing 5 pulse stimulation with the other 4 conditions.
MEP latencies were significantly longer for both 2 + 7 and 4 + 5 pulse stimulations compared with either 5, 7 and 9 pulse stimulation bilaterally. This was observed in the upper and lower limb recordings.
CSM is known to result in cortical reorganization both before and after decompression surgery (Green t al, 2015). Our findings suggest that the temporal priming effects of double train stimulation may be negated in severe CSM at the cortical or spinal levels. Thus, the use of differential cortical stimulating positions should be explored as a spatial modifying strategy.
- Time
- Topic
- Speaker
- Moderator
- 09:30-10:00
- Assessment of brain connectivity from cortico-cortical evoked potentials
- Speaker:
Szu-Yen PAN
- Moderator:
Jin-An Huang
- Szu-Yen PAN
- MD
-
Attending physician, Departement of Neurosurgery, Neurological Institute, Taichung Veterans General Hospital
Department of Post-Baccalaureate Medicine, College of Medicine, National Chung Hsing University
E-mail:moongrace.tw@gmail.com
Executive Summary:
Dr. Szu-Yen Pan is a neurosurgeon and clinical neurophysiologist at Taichung Veterans General Hospital in Taiwan, distinguished for her work in functional neurosurgery and intraoperative neurophysiological monitoring. She completed her medical degree at Chung Shan Medical University, followed by neurosurgical residency and chief residency training at Taichung VGH. Dr. Pan further broadened her expertise through a clinical fellowship at the Centre Hospitalier Universitaire Grenoble Alpes in France and later as a visiting scholar at the University of California, San Francisco, where she received advanced training in IONM and perioperative neuromonitoring.
Her academic and clinical contributions span facial motor evoked potentials, cranial nerve preservation strategies during cerebellopontine angle tumor surgery, and tailored neuromonitoring techniques for glioma resection. She has published in leading journals such as Neurosurgical Focus, Clinical Neurophysiology, and the Journal of Neuro-Oncology. In 2024, she was honored with the Top Scientific Achievement Award from the American Society of Neurophysiological Monitoring in recognition of her innovative work.
Dr. Szu-Yen Pan is a neurosurgeon and clinical neurophysiologist at Taichung Veterans General Hospital in Taiwan, distinguished for her work in functional neurosurgery and intraoperative neurophysiological monitoring. She completed her medical degree at Chung Shan Medical University, followed by neurosurgical residency and chief residency training at Taichung VGH. Dr. Pan further broadened her expertise through a clinical fellowship at the Centre Hospitalier Universitaire Grenoble Alpes in France and later as a visiting scholar at the University of California, San Francisco, where she received advanced training in IONM and perioperative neuromonitoring.
Her academic and clinical contributions span facial motor evoked potentials, cranial nerve preservation strategies during cerebellopontine angle tumor surgery, and tailored neuromonitoring techniques for glioma resection. She has published in leading journals such as Neurosurgical Focus, Clinical Neurophysiology, and the Journal of Neuro-Oncology. In 2024, she was honored with the Top Scientific Achievement Award from the American Society of Neurophysiological Monitoring in recognition of her innovative work.
Lecture Abstract:
Cortico-cortical evoked potentials (CCEPs) have progressed over the past two decades from an invasive research tool used primarily in extraoperative epilepsy studies to a promising intraoperative modality for functional brain mapping. Early foundational work established CCEPs as a method for probing effective connectivity through single-pulse electrical stimulation, revealing dynamic interactions across language, motor, sensory, and associative networks. More recently, intraoperative adaptations have extended their applicability to neuro-oncological surgery, enabling surgeons to evaluate large-scale cortical networks under general anesthesia when traditional awake mapping is not feasible.
Our current work represents the beginning of a broader effort to translate these advances into practical clinical use. At this stage, our investigations focus on individual patient cases, integrating CCEPs with multimodal imaging and standard neurophysiological monitoring to understand how brain tumors—and tumor-related epilepsy—alter functional connectivity. Through early-case observations, we have begun to document variations in N1/N2 characteristics, connectivity asymmetries, and dynamic changes during tumor manipulation. These case-based findings offer preliminary insight into network reorganization and the potential role of CCEPs in predicting functional vulnerability.
As our research is in its initial phase, the goal of this presentation is not to present definitive conclusions, but rather to illustrate how early application of CCEPs can enrich our understanding of individualized brain networks and guide future systematic studies. By sharing these initial experiences, we aim to contribute to the ongoing evolution of CCEP methodology and its future integration into personalized neurosurgical planning.
Cortico-cortical evoked potentials (CCEPs) have progressed over the past two decades from an invasive research tool used primarily in extraoperative epilepsy studies to a promising intraoperative modality for functional brain mapping. Early foundational work established CCEPs as a method for probing effective connectivity through single-pulse electrical stimulation, revealing dynamic interactions across language, motor, sensory, and associative networks. More recently, intraoperative adaptations have extended their applicability to neuro-oncological surgery, enabling surgeons to evaluate large-scale cortical networks under general anesthesia when traditional awake mapping is not feasible.
Our current work represents the beginning of a broader effort to translate these advances into practical clinical use. At this stage, our investigations focus on individual patient cases, integrating CCEPs with multimodal imaging and standard neurophysiological monitoring to understand how brain tumors—and tumor-related epilepsy—alter functional connectivity. Through early-case observations, we have begun to document variations in N1/N2 characteristics, connectivity asymmetries, and dynamic changes during tumor manipulation. These case-based findings offer preliminary insight into network reorganization and the potential role of CCEPs in predicting functional vulnerability.
As our research is in its initial phase, the goal of this presentation is not to present definitive conclusions, but rather to illustrate how early application of CCEPs can enrich our understanding of individualized brain networks and guide future systematic studies. By sharing these initial experiences, we aim to contribute to the ongoing evolution of CCEP methodology and its future integration into personalized neurosurgical planning.
- Time
- Topic
- Speaker
- Moderator
- 10:30-11:00
- IONM of cognitive function in waking status: the experience from intra-axial glioma treatment
- Speaker:
Wei-Han Chang
- Moderator:
Peng-Wei Hsu
- Wei-Han Chang
- M.D., PhD.
-
Department Director, Department of Physical Medicine and Rehabilitation, Chang Gung Memorial Hospital at Keelung
Assistant Professor, School of Traditional Chinese Medicine, Chang Gung University
E-mail:m7252@cgmh.org.tw
Executive Summary:
1. Department Director, Department of Physical medicine and rehabilitation, Chang Gung Memorial Hospital at Keelung, Keelung.
2. The clinical assistant professor of School of Tranditional Chinese Medicine, Chang Gung University.
Research Interest:
1. Functional mapping of language and other eloquent areas in awake craniotomy
2. Assessments of dysphagia and dysphagia treatment
3. Neuroscience and neurorehabilitation
1. Department Director, Department of Physical medicine and rehabilitation, Chang Gung Memorial Hospital at Keelung, Keelung.
2. The clinical assistant professor of School of Tranditional Chinese Medicine, Chang Gung University.
Research Interest:
1. Functional mapping of language and other eloquent areas in awake craniotomy
2. Assessments of dysphagia and dysphagia treatment
3. Neuroscience and neurorehabilitation
Lecture Abstract:
Awake craniotomy is a form of intraoperative neurophysiological monitoring (IONM). It allows for the monitoring of various cognitive functions of the brain, among which language is the most commonly assessed function. Language processing is thought to be governed by two neural networks: the dorsal stream and the ventral stream. Brain tumors located near language areas may compress or disrupt these networks, leading to language impairments and triggering reorganization of the networks (neuroplasticity). Therefore, patients with brain tumors in language-related regions provide an excellent model for studying language networks and their neuroplasticity. Our research approaches this topic from the perspective of functional language assessment. This presentation will share the research findings on the recovery potential after language impairments, how patient and tumor characteristics influence the neuroplasticity of language functions, and exploring the classification of language networks from a functional assessment perspective.
Awake craniotomy is a form of intraoperative neurophysiological monitoring (IONM). It allows for the monitoring of various cognitive functions of the brain, among which language is the most commonly assessed function. Language processing is thought to be governed by two neural networks: the dorsal stream and the ventral stream. Brain tumors located near language areas may compress or disrupt these networks, leading to language impairments and triggering reorganization of the networks (neuroplasticity). Therefore, patients with brain tumors in language-related regions provide an excellent model for studying language networks and their neuroplasticity. Our research approaches this topic from the perspective of functional language assessment. This presentation will share the research findings on the recovery potential after language impairments, how patient and tumor characteristics influence the neuroplasticity of language functions, and exploring the classification of language networks from a functional assessment perspective.
- Time
- Topic
- Speaker
- Moderator
- 11:00-11:30
- Functional neurophysiological navigation of surgery guidance of skull brain tumor
- Speaker:
Cheng-Chia Lee
- Moderator:
Chun-Fu Lin
- Cheng-Chia Lee
- MD, PhD
-
Visiting staff, Department of Neurosurgery, Taipei Veterans General Hospital
E-mail:yfnaughty@gmail.com
Executive Summary:
Dr. Lee is a functional neurosurgeon at Taipei Veteran General Hospital, who specializes in Gamma Knife radiosurgery, epilepsy surgery, interventional pain management, and intra-operative neuromonitoring. His research interests mainly focus on epilepsy network, EEG signal analysis, and radiation effects after Gamma knife radiosurgery. Now, Dr. Lee is a member of epilepsy surgery team in Taipei VGH, and extremely professional in field of stereo-EEG (SEEG) planning and implantation. He completed his fellowship in Department of Neurological Surgery, University of Virginia on 2013-14. Since 2014, he got several awards including Outstanding Paper Award from Taiwan Neurosurgerical Society, Young Researcher Scholarship from Taiwan Epilepsy Society, Young Researcher Scholarship from Taiwan Pain Society, and Young Neurosurgery Award (Top 15) from World Federation of Neurosurgical Societies (WFNS). Until now, he has published 160 articles and 68 international conference pape
Dr. Lee is a functional neurosurgeon at Taipei Veteran General Hospital, who specializes in Gamma Knife radiosurgery, epilepsy surgery, interventional pain management, and intra-operative neuromonitoring. His research interests mainly focus on epilepsy network, EEG signal analysis, and radiation effects after Gamma knife radiosurgery. Now, Dr. Lee is a member of epilepsy surgery team in Taipei VGH, and extremely professional in field of stereo-EEG (SEEG) planning and implantation. He completed his fellowship in Department of Neurological Surgery, University of Virginia on 2013-14. Since 2014, he got several awards including Outstanding Paper Award from Taiwan Neurosurgerical Society, Young Researcher Scholarship from Taiwan Epilepsy Society, Young Researcher Scholarship from Taiwan Pain Society, and Young Neurosurgery Award (Top 15) from World Federation of Neurosurgical Societies (WFNS). Until now, he has published 160 articles and 68 international conference pape
Lecture Abstract:
Surgical management of skull base brain tumors poses significant challenges due to their proximity to critical neurovascular structures and functional brain regions. Functional neurophysiological navigation—integrating techniques such as intraoperative neurophysiological monitoring (IONM), direct cortical and subcortical stimulation, motor-evoked potentials (MEPs), somatosensory-evoked potentials (SSEPs), and brain mapping—has emerged as a crucial tool in guiding safe and effective resections. These techniques enable real-time identification and preservation of eloquent cortex and cranial nerve pathways, enhancing surgical precision while reducing the risk of postoperative deficits. This approach represents a paradigm shift toward functional preservation in skull base tumor surgery, contributing to improved neurological and oncological outcomes.
Surgical management of skull base brain tumors poses significant challenges due to their proximity to critical neurovascular structures and functional brain regions. Functional neurophysiological navigation—integrating techniques such as intraoperative neurophysiological monitoring (IONM), direct cortical and subcortical stimulation, motor-evoked potentials (MEPs), somatosensory-evoked potentials (SSEPs), and brain mapping—has emerged as a crucial tool in guiding safe and effective resections. These techniques enable real-time identification and preservation of eloquent cortex and cranial nerve pathways, enhancing surgical precision while reducing the risk of postoperative deficits. This approach represents a paradigm shift toward functional preservation in skull base tumor surgery, contributing to improved neurological and oncological outcomes.
- Time
- Topic
- Speaker
- Moderator
- 11:30-12:00
- How to monitor surgeries of spinal cord tumor and disorders?
- Speaker:
Paulo Andre Teixeira Kimaid
- Moderator:
Jimmy Ming-Jung Chuang
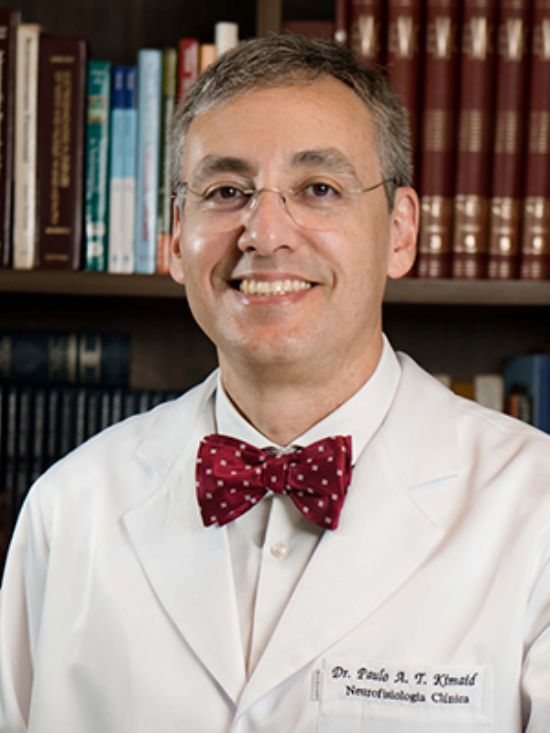
- Paulo Andre Teixeira Kimaid
- MD, PhD
-
Head of Evoked Potential and Intraoperative Neuromonitoring Division , CENEC - Neurofisiologia Clínica
Head of Intraoperative Neuromonitoring , University of Campinas - UNICAMP
E-mail:paulokimaid@yahoo.com.br
Executive Summary:
Professor Paulo Kimaid, MD, PhD is a Board-Certified Neurologist and Clinical Neurophysiologist in Brazil. He has a master’s degree in sciences and a professional doctorate in Medical Sciences, area of Neurology. He is a Past-President of the Brazilian Society of Clinical Neurophysiology and a Past-President of the Latin America Chapter of the IFCN. He is a Director of the Exxecutive Committee and the Co-chair of the Education Committee of the IFCN. He is interested in both education and clinical practice. His clinical interests are peripheral nerve neurophysiology and imaging, evoked potentials and intraoperative neurophysiology.
Professor Paulo Kimaid, MD, PhD is a Board-Certified Neurologist and Clinical Neurophysiologist in Brazil. He has a master’s degree in sciences and a professional doctorate in Medical Sciences, area of Neurology. He is a Past-President of the Brazilian Society of Clinical Neurophysiology and a Past-President of the Latin America Chapter of the IFCN. He is a Director of the Exxecutive Committee and the Co-chair of the Education Committee of the IFCN. He is interested in both education and clinical practice. His clinical interests are peripheral nerve neurophysiology and imaging, evoked potentials and intraoperative neurophysiology.
Lecture Abstract:
Intraoperative neuromonitoring (IONM) has emerged as a useful tool in spinal surgery, offering real-time assessment of neural integrity and significantly enhancing surgical precision and patient outcomes. This review explores the role and utility of IONM across procedures involving spinal tumors and other spinal pathologies. Spinal tumors—both intramedullary and extramedullary pose challenges due to their proximity to critical neural structures. Techniques such as somatosensory evoked potentials (SSEP), motor evoked potentials (MEP) and electromyography (EMG) provide early warning signs of potential neural compromise, allowing surgeons to adjust their approach intraoperatively to preserve function. Also, dorsal columns and corticospinal tract mapping offer precise location of these structures guiding the surgeons during tumor resection. Additionally, IONM has proven beneficial in surgeries for spinal deformities, disc herniation, tethered cord syndrome, and degenerative conditions. Evidence from multicenter studies suggests that IONM reduces the incidence of postoperative neurological deficits and aids in intraoperative decision-making. Challenges remain in standardizing protocols, interpreting signals in real time, and integrating IONM across varying surgical teams. Future directions emphasize enhanced signal interpretation through artificial intelligence, multimodal integration, and better accessibility in resource-limited settings. As spinal surgery continues to evolve, IONM stands as a cornerstone of neuroprotection, looking for optimal outcomes and expanding the boundaries of what is safely achievable. This review underscores IONM’s role in spine surgery and calls for continued research to refine its application.
Intraoperative neuromonitoring (IONM) has emerged as a useful tool in spinal surgery, offering real-time assessment of neural integrity and significantly enhancing surgical precision and patient outcomes. This review explores the role and utility of IONM across procedures involving spinal tumors and other spinal pathologies. Spinal tumors—both intramedullary and extramedullary pose challenges due to their proximity to critical neural structures. Techniques such as somatosensory evoked potentials (SSEP), motor evoked potentials (MEP) and electromyography (EMG) provide early warning signs of potential neural compromise, allowing surgeons to adjust their approach intraoperatively to preserve function. Also, dorsal columns and corticospinal tract mapping offer precise location of these structures guiding the surgeons during tumor resection. Additionally, IONM has proven beneficial in surgeries for spinal deformities, disc herniation, tethered cord syndrome, and degenerative conditions. Evidence from multicenter studies suggests that IONM reduces the incidence of postoperative neurological deficits and aids in intraoperative decision-making. Challenges remain in standardizing protocols, interpreting signals in real time, and integrating IONM across varying surgical teams. Future directions emphasize enhanced signal interpretation through artificial intelligence, multimodal integration, and better accessibility in resource-limited settings. As spinal surgery continues to evolve, IONM stands as a cornerstone of neuroprotection, looking for optimal outcomes and expanding the boundaries of what is safely achievable. This review underscores IONM’s role in spine surgery and calls for continued research to refine its application.