Time slot's time in Taipei (GMT+8)
2025/11/21 14:00-17:30 Room 101 CD
- Kick-on Seminar VI
Evoked Potential: New Perspectives from the Old Tales for Advancing Applications in Real World
- Time
- Topic
- Speaker
- Moderator
- 14:00-14:30
- Visual evoked potentials as neurophysiological markers for understanding migraine
- Speaker:
Chi ieong David Lau
- Moderator:
Wei-Hung Chen
- Chi ieong David Lau
- MD, PhD
-
Director/Consultant Neurologist, Dementia Center, Department of Neurology, Shin Kong Wu Ho-Su Memorial Hospital, Taipei, Taiwan
Assistant Professor, 1) Institute of Biophotonics, National Yang-Ming Chiao Tung University; 2) College of Medicine, Fu-Jen Catholic University
Director of Board, Taiwan Headache Society
E-mail:drlauci@gmail.com
Executive Summary:
Dr Chi ieong David Lau(劉) is a consultant neurologist and Director of the Dementia Centre at Shin-Kong Wu Ho-Su Memorial Hospital, Taipei, and Assistant Professor at National Yang Ming Chiao Tung University and Fu Jen Catholic University. A British Chevening Scholar, he earned a PhD and MSc from University College London, Queen Square, and an MSc from the University of Oxford, following his medical degree and neurology training in Taiwan. He has published over 40 SCI-indexed papers in Neurology, Headache, Cephalalgia, Brain Stimulation and other leading journals.
His expertise spans three main areas:
1. Non-invasive brain stimulation – Pioneered the use of transcranial direct current stimulation (tDCS) to disrupt memory consolidation during sleep, demonstrated additive benefits of multi-session tDCS with Tai Chi and computerised training on gait and executive function in mild cognitive impairment (MCI), and explored cortical excitability modulation in migraine. Co-founder of the Taiwan Brain Stimulation Society.
2. Headache disorders – Former Secretary-General and current Board Director of the Taiwan Headache Society, first author of the 2022 Taiwan Guidelines for Acute Treatment of Migraine (update in progress). Conducted behavioural studies on decision-making impairments in medication overuse headache (MOH), nationwide cohort studies linking migraine to systemic comorbidities, and AI-driven neuroimaging to study migraine brain morphology.
3. Neurodegenerative diseases – Leads MRI projects with over 1,000 participants, developing AI-enhanced models to detect early brain network changes and estimate brain age, including studies on executive function in MCI.
Integrating neuroimaging, brain stimulation and big-data analytics, Dr Lau develops precision tools for the early detection and treatment of brain disorders.
Dr Chi ieong David Lau(劉) is a consultant neurologist and Director of the Dementia Centre at Shin-Kong Wu Ho-Su Memorial Hospital, Taipei, and Assistant Professor at National Yang Ming Chiao Tung University and Fu Jen Catholic University. A British Chevening Scholar, he earned a PhD and MSc from University College London, Queen Square, and an MSc from the University of Oxford, following his medical degree and neurology training in Taiwan. He has published over 40 SCI-indexed papers in Neurology, Headache, Cephalalgia, Brain Stimulation and other leading journals.
His expertise spans three main areas:
1. Non-invasive brain stimulation – Pioneered the use of transcranial direct current stimulation (tDCS) to disrupt memory consolidation during sleep, demonstrated additive benefits of multi-session tDCS with Tai Chi and computerised training on gait and executive function in mild cognitive impairment (MCI), and explored cortical excitability modulation in migraine. Co-founder of the Taiwan Brain Stimulation Society.
2. Headache disorders – Former Secretary-General and current Board Director of the Taiwan Headache Society, first author of the 2022 Taiwan Guidelines for Acute Treatment of Migraine (update in progress). Conducted behavioural studies on decision-making impairments in medication overuse headache (MOH), nationwide cohort studies linking migraine to systemic comorbidities, and AI-driven neuroimaging to study migraine brain morphology.
3. Neurodegenerative diseases – Leads MRI projects with over 1,000 participants, developing AI-enhanced models to detect early brain network changes and estimate brain age, including studies on executive function in MCI.
Integrating neuroimaging, brain stimulation and big-data analytics, Dr Lau develops precision tools for the early detection and treatment of brain disorders.
Lecture Abstract:
Finding a reliable biomarker to diagnose migraine remains a major challenge in the headache field. Migraine patients exhibit dynamic and recurrent alterations in the brainstem–thalamo–cortical loop, including reduced thalamocortical activity and abnormal habituation during the interictal phase. These insights have advanced our understanding of migraine pathophysiology, yet no such measures are currently implemented in clinical practice.
Habituation—the progressive reduction in neural response to repeated stimulation—is a fundamental adaptive process that prevents cortical overload. In healthy individuals, visual evoked potentials (VEPs) typically decline in amplitude during continuous pattern-reversal stimulation. In many migraineurs, however, interictal VEPs show deficient habituation or even potentiation, often with lower initial amplitudes, suggesting reduced cortical pre-activation and altered thalamo-cortical regulation. This deficit is not static: it worsens in the days before an attack, normalises peri-ictally, and reappears post-ictally. Similar patterns are observed in auditory, somatosensory, and nociceptive modalities, supporting the thalamo-cortical dysrhythmia model. Yet replication has been inconsistent, with methodological and patient-selection factors likely contributing to variability.
Non-invasive brain stimulation has been explored as a means to modulate these neurophysiological patterns. Transcranial direct current stimulation (tDCS) over the visual cortex is of particular interest for potentially restoring normal habituation. In a small proof-of-concept crossover study (Lau et al., 2021, Neuroscience Letters; Lau et al., 2020, Progress in Brain Research), we applied anodal, cathodal, and sham tDCS to healthy participants and assessed VEP amplitudes and habituation slopes before and after stimulation. No polarity-specific after-effects were detected, suggesting that motor-derived tDCS models may not directly apply to the visual system.
VEP habituation remains a promising but debated candidate biomarker for migraine. Establishing its reliability, clinical utility, and modifiability will require standardised protocols, large-scale longitudinal studies, and integration with other neurophysiological and imaging markers.
Finding a reliable biomarker to diagnose migraine remains a major challenge in the headache field. Migraine patients exhibit dynamic and recurrent alterations in the brainstem–thalamo–cortical loop, including reduced thalamocortical activity and abnormal habituation during the interictal phase. These insights have advanced our understanding of migraine pathophysiology, yet no such measures are currently implemented in clinical practice.
Habituation—the progressive reduction in neural response to repeated stimulation—is a fundamental adaptive process that prevents cortical overload. In healthy individuals, visual evoked potentials (VEPs) typically decline in amplitude during continuous pattern-reversal stimulation. In many migraineurs, however, interictal VEPs show deficient habituation or even potentiation, often with lower initial amplitudes, suggesting reduced cortical pre-activation and altered thalamo-cortical regulation. This deficit is not static: it worsens in the days before an attack, normalises peri-ictally, and reappears post-ictally. Similar patterns are observed in auditory, somatosensory, and nociceptive modalities, supporting the thalamo-cortical dysrhythmia model. Yet replication has been inconsistent, with methodological and patient-selection factors likely contributing to variability.
Non-invasive brain stimulation has been explored as a means to modulate these neurophysiological patterns. Transcranial direct current stimulation (tDCS) over the visual cortex is of particular interest for potentially restoring normal habituation. In a small proof-of-concept crossover study (Lau et al., 2021, Neuroscience Letters; Lau et al., 2020, Progress in Brain Research), we applied anodal, cathodal, and sham tDCS to healthy participants and assessed VEP amplitudes and habituation slopes before and after stimulation. No polarity-specific after-effects were detected, suggesting that motor-derived tDCS models may not directly apply to the visual system.
VEP habituation remains a promising but debated candidate biomarker for migraine. Establishing its reliability, clinical utility, and modifiability will require standardised protocols, large-scale longitudinal studies, and integration with other neurophysiological and imaging markers.
- Time
- Topic
- Speaker
- Moderator
- 14:30-15:00
- Somatosensory evoked potentials (SSEP): a promising biomarker for chronic pain syndrome
- Speaker:
Chi-Chao Chao
- Moderator:
Sung-Tsang Hsieh
- Chi-Chao Chao
- MD, PhD.
-
Director, Neuromuscular Division, Department of Neurology, National Taiwan University Hospital
E-mail:ccchao@ntu.edu.tw
Executive Summary:
Chi-Chao Chao is an attending neurologist in the Department of Neurology at National Taiwan University Hospital, Taipei, Taiwan. Dr. Chao graduated with his medical degree at the National Taiwan University School of Medicine, and received his PhD training from the National Taiwan University College of Medicine Graduate Institute of Clinical Medicine. He completed his residency in the Department of Neurology at National Taiwan University Hospital and was a Postdoctoral Research Fellow at the Humor Motor Control Section of the National Institute of Health, USA, from 2011-2012. Dr. Chao’s research interests are clinical neurophysiology, peripheral neuropathy and neuropathic pain. He has applied pathologic and physiological tools to explore the pathophysiology of variable neuropathic disorders and dissect the mechanism of peripheral and central neuropathic pain.
Chi-Chao Chao is an attending neurologist in the Department of Neurology at National Taiwan University Hospital, Taipei, Taiwan. Dr. Chao graduated with his medical degree at the National Taiwan University School of Medicine, and received his PhD training from the National Taiwan University College of Medicine Graduate Institute of Clinical Medicine. He completed his residency in the Department of Neurology at National Taiwan University Hospital and was a Postdoctoral Research Fellow at the Humor Motor Control Section of the National Institute of Health, USA, from 2011-2012. Dr. Chao’s research interests are clinical neurophysiology, peripheral neuropathy and neuropathic pain. He has applied pathologic and physiological tools to explore the pathophysiology of variable neuropathic disorders and dissect the mechanism of peripheral and central neuropathic pain.
Lecture Abstract:
Abstract:
Chronic pain syndrome is defined as chronic persistent pain lasting outlasting longer normal tissue healing. Chronic pain syndrome encompasses not only nociceptive process but also neuropathic mechanism, and is associated with central sensitization, altered pain modulation, psychological distress, sleep disturbance, and functional disability, making it a biopsychosocial condition. Chronic pain syndrome poses major diagnostic and therapeutic challenges for physicians, highlighting the urgent need for reliable biomarkers and multidisciplinary management. Usually the diagnosis of chronic pain syndrome relies almost entirely on subjective patient reports and there is no objective biomarker or gold-standard test. Somatosensory evoked potential records cortical responses to electric stimulation of large Aβ fibers or to painful stimulation of unmyelinated (C) or thinly myelinated (Aδ) fibers, and can serve as a tool to detect lesions in somatosensory pathways. It has been proved useful in the diagnosis of peripheral neuropathy involving the sensory nerves, myelopathy affecting sensory afferent tracts and brain disorders with somatosenosry netword dysfunction. More recent studies also showed the pain evoked potential could explore the underlying pathophysiological mechanisms of neuropathic pain. In the lecture, I will introduce the electrophysiology and neuroimage evoked by somatosensory stimuli and their clinical applications in chronic pain syndrome.
Abstract:
Chronic pain syndrome is defined as chronic persistent pain lasting outlasting longer normal tissue healing. Chronic pain syndrome encompasses not only nociceptive process but also neuropathic mechanism, and is associated with central sensitization, altered pain modulation, psychological distress, sleep disturbance, and functional disability, making it a biopsychosocial condition. Chronic pain syndrome poses major diagnostic and therapeutic challenges for physicians, highlighting the urgent need for reliable biomarkers and multidisciplinary management. Usually the diagnosis of chronic pain syndrome relies almost entirely on subjective patient reports and there is no objective biomarker or gold-standard test. Somatosensory evoked potential records cortical responses to electric stimulation of large Aβ fibers or to painful stimulation of unmyelinated (C) or thinly myelinated (Aδ) fibers, and can serve as a tool to detect lesions in somatosensory pathways. It has been proved useful in the diagnosis of peripheral neuropathy involving the sensory nerves, myelopathy affecting sensory afferent tracts and brain disorders with somatosenosry netword dysfunction. More recent studies also showed the pain evoked potential could explore the underlying pathophysiological mechanisms of neuropathic pain. In the lecture, I will introduce the electrophysiology and neuroimage evoked by somatosensory stimuli and their clinical applications in chronic pain syndrome.
- Time
- Topic
- Speaker
- Moderator
- 15:00-15:30
- Uncommon SSEP studies in clinical common disease
- Speaker:
Paulo Andre Teixeira Kimaid
- Moderator:
Zin-An Wu
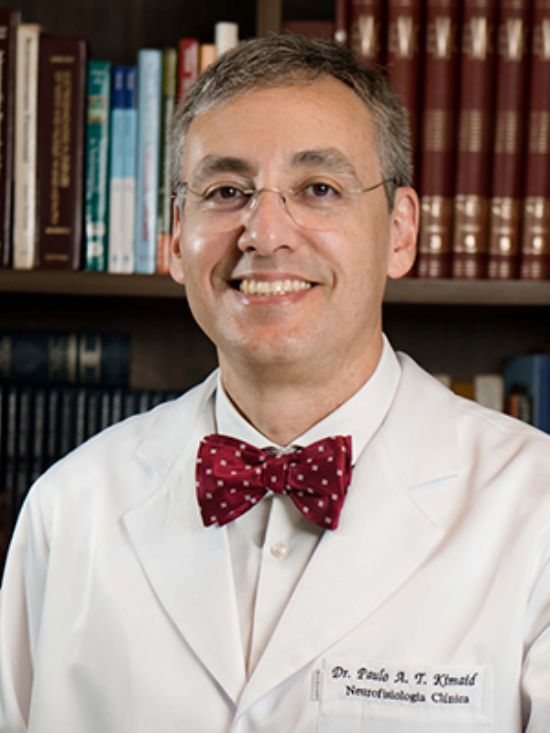
- Paulo Andre Teixeira Kimaid
- MD, PhD
-
Head of Evoked Potential and Intraoperative Neuromonitoring Division , CENEC - Neurofisiologia Clínica
Head of Intraoperative Neuromonitoring , University of Campinas - UNICAMP
E-mail:paulokimaid@yahoo.com.br
Executive Summary:
Professor Paulo Kimaid, MD, PhD is a Board-Certified Neurologist and Clinical Neurophysiologist in Brazil. He has a master’s degree in sciences and a professional doctorate in Medical Sciences, area of Neurology. He is a Past-President of the Brazilian Society of Clinical Neurophysiology and a Past-President of the Latin America Chapter of the IFCN. He is a Director of the Exxecutive Committee and the Co-chair of the Education Committee of the IFCN. He is interested in both education and clinical practice. His clinical interests are peripheral nerve neurophysiology and imaging, evoked potentials and intraoperative neurophysiology.
Professor Paulo Kimaid, MD, PhD is a Board-Certified Neurologist and Clinical Neurophysiologist in Brazil. He has a master’s degree in sciences and a professional doctorate in Medical Sciences, area of Neurology. He is a Past-President of the Brazilian Society of Clinical Neurophysiology and a Past-President of the Latin America Chapter of the IFCN. He is a Director of the Exxecutive Committee and the Co-chair of the Education Committee of the IFCN. He is interested in both education and clinical practice. His clinical interests are peripheral nerve neurophysiology and imaging, evoked potentials and intraoperative neurophysiology.
Lecture Abstract:
Somatosensory evoked potentials (SSEPs) are a valuable diagnostic modality for evaluating the functional integrity of sensory pathways. While most clinical applications focus on commonly stimulated nerves such as median and tibial, emerging interest in utilizing SSEPs from less frequently assessed nerves — including the genitofemoral, pudendal, intercostobrachial, inferior alveolar and lingual — has demonstrated promising diagnostic potential. This lecture explores the clinical relevance of recording SSEPs from these atypical sites. Uncommon nerve SSEPs can complement standard protocols when evaluating focal neuropathies or entrapment syndromes with nerve conduction studies is limited or not possible. Incorporating uncommon nerve recordings can add objectivity to the diagnostic workup. Despite the challenges, such as lower signal amplitudes and greater susceptibility to artifacts, advancements in stimulation and recording techniques have improved reliability. Clinicians must tailor protocols to individual patient complaints. Overall, SSEPs from uncommon nerves are underutilized but can become very good tools in the neurophysiological arsenal, expanding the diagnostic horizon, especially peripheral sensory dysfunction and enhancing clinical decision-making.
Somatosensory evoked potentials (SSEPs) are a valuable diagnostic modality for evaluating the functional integrity of sensory pathways. While most clinical applications focus on commonly stimulated nerves such as median and tibial, emerging interest in utilizing SSEPs from less frequently assessed nerves — including the genitofemoral, pudendal, intercostobrachial, inferior alveolar and lingual — has demonstrated promising diagnostic potential. This lecture explores the clinical relevance of recording SSEPs from these atypical sites. Uncommon nerve SSEPs can complement standard protocols when evaluating focal neuropathies or entrapment syndromes with nerve conduction studies is limited or not possible. Incorporating uncommon nerve recordings can add objectivity to the diagnostic workup. Despite the challenges, such as lower signal amplitudes and greater susceptibility to artifacts, advancements in stimulation and recording techniques have improved reliability. Clinicians must tailor protocols to individual patient complaints. Overall, SSEPs from uncommon nerves are underutilized but can become very good tools in the neurophysiological arsenal, expanding the diagnostic horizon, especially peripheral sensory dysfunction and enhancing clinical decision-making.
- Time
- Topic
- Speaker
- Moderator
- 16:00-16:30
- The Evolving Role of Evoked Potentials in Neuroprognostication
- Speaker:
Aatif Mairaj Husain
- Moderator:
Mark Anthony J Sta Maria
- Aatif Mairaj Husain
- MD
-
Chief, Division of Epilepsy, Sleep, and Clinical Neurophysiology, Duke University
E-mail:aatif.husain@duke.edu
Executive Summary:
Dr. Aatif Husain is a Professor in the Department of Neurology and Chief of the Division of Epilepsy, Sleep, and Clinical Neurophysiology at Duke University Medical Center in Durham, North Carolina. He also serves as Co-Director of the Neuroscience Clinical Services Unit at Duke University Hospital.
He is currently the Treasurer of the International Federation of Clinical Neurophysiology and Chair of the Council of Clinical Activities of the American Epilepsy Society. Dr. Husain is a past President of both the American Clinical Neurophysiology Society and ABRET and has previously served as Editor-in-Chief of the Journal of Clinical Neurophysiology.
His clinical and research interests focus on evoked potentials, neurophysiologic intraoperative monitoring, and the treatment of acute seizures, status epilepticus, narcolepsy, and other hypersomnias.
Dr. Aatif Husain is a Professor in the Department of Neurology and Chief of the Division of Epilepsy, Sleep, and Clinical Neurophysiology at Duke University Medical Center in Durham, North Carolina. He also serves as Co-Director of the Neuroscience Clinical Services Unit at Duke University Hospital.
He is currently the Treasurer of the International Federation of Clinical Neurophysiology and Chair of the Council of Clinical Activities of the American Epilepsy Society. Dr. Husain is a past President of both the American Clinical Neurophysiology Society and ABRET and has previously served as Editor-in-Chief of the Journal of Clinical Neurophysiology.
His clinical and research interests focus on evoked potentials, neurophysiologic intraoperative monitoring, and the treatment of acute seizures, status epilepticus, narcolepsy, and other hypersomnias.
Lecture Abstract:
Evoked potentials (EPs) have become a valuable tool in neuroprognostication, particularly in comatose patients following acute brain injuries such as cardiac arrest, traumatic brain injury, and stroke. By assessing the integrity of sensory pathways, EPs offer an objective, non-invasive measure of brain function when clinical examination is limited. Somatosensory evoked potentials (SEPs), especially short-latency responses, are widely used for predicting poor outcomes, as their absence is strongly associated with a lack of meaningful neurologic recovery. Middle latency SEPs can provide additional insights into cortical function but are less commonly applied.
On the other hand, the presence of specific auditory evoked responses, such as the mismatch negativity (MMN) and the novelty P3 component, has shown promise in predicting good neurologic outcomes. These event-related potentials reflect higher-order cortical processing, suggesting preserved cognitive pathways and potential for recovery. Emerging data suggests that SEP amplitude may also help in prognosticating favorable outcomes.
The evolving role of EPs lies in their integration with multimodal prognostic tools, including EEG, imaging, and biomarkers. Advances in signal analysis and machine learning may further enhance their predictive accuracy. As clinical protocols increasingly emphasize individualized care, evoked potentials offer a repeatable, bedside-accessible measure that supports more confident and early decision-making in neurocritical care settings.
Evoked potentials (EPs) have become a valuable tool in neuroprognostication, particularly in comatose patients following acute brain injuries such as cardiac arrest, traumatic brain injury, and stroke. By assessing the integrity of sensory pathways, EPs offer an objective, non-invasive measure of brain function when clinical examination is limited. Somatosensory evoked potentials (SEPs), especially short-latency responses, are widely used for predicting poor outcomes, as their absence is strongly associated with a lack of meaningful neurologic recovery. Middle latency SEPs can provide additional insights into cortical function but are less commonly applied.
On the other hand, the presence of specific auditory evoked responses, such as the mismatch negativity (MMN) and the novelty P3 component, has shown promise in predicting good neurologic outcomes. These event-related potentials reflect higher-order cortical processing, suggesting preserved cognitive pathways and potential for recovery. Emerging data suggests that SEP amplitude may also help in prognosticating favorable outcomes.
The evolving role of EPs lies in their integration with multimodal prognostic tools, including EEG, imaging, and biomarkers. Advances in signal analysis and machine learning may further enhance their predictive accuracy. As clinical protocols increasingly emphasize individualized care, evoked potentials offer a repeatable, bedside-accessible measure that supports more confident and early decision-making in neurocritical care settings.
- Time
- Topic
- Speaker
- Moderator
- 16:30-17:00
- TMS evoked EEG potentials: technique, interpretation and clinical applications
- Speaker:
Po-Yu Fong
- Moderator:
Wen-Li Chuang
- Po-Yu Fong
- MD PhD
-
Consultant Neurologist, Chang Gung Memorial Hospital, Linkou Branch
E-mail:neurologist.fong@gmail.com
Executive Summary:
Dr Po-Yu Fong is a consultant neurologist at Chang Gung Memorial Hospital, Linkou, specialising in movement disorders, electrophysiology, and non-invasive brain stimulation. After completing medical training at Chung Shan Medical University and residency at CGMH, he earned his PhD at the UCL Queen Square Institute of Neurology, where he investigated cortical physiology using TMS–EEG co-registration.
His academic focus lies in TMS, rTMS, and EEG, with applications in both research and clinical settings. He currently leads the rTMS treatment team at CGMH and trains residents in neuromodulation. As Secretary General of the Taiwan Movement Disorder Society, he coordinates educational programmes and fosters collaborations. His goal is to advance neuromodulation as a therapeutic tool in neurology and psychiatry.
Dr Po-Yu Fong is a consultant neurologist at Chang Gung Memorial Hospital, Linkou, specialising in movement disorders, electrophysiology, and non-invasive brain stimulation. After completing medical training at Chung Shan Medical University and residency at CGMH, he earned his PhD at the UCL Queen Square Institute of Neurology, where he investigated cortical physiology using TMS–EEG co-registration.
His academic focus lies in TMS, rTMS, and EEG, with applications in both research and clinical settings. He currently leads the rTMS treatment team at CGMH and trains residents in neuromodulation. As Secretary General of the Taiwan Movement Disorder Society, he coordinates educational programmes and fosters collaborations. His goal is to advance neuromodulation as a therapeutic tool in neurology and psychiatry.
Lecture Abstract:
TMS and EEG co-registration (TMS-EEG) is a newly developed technique to record the post-synaptic potential on the cortex evoked by TMS. TMS-EEG provides more information on cortical physiology than conventional motor-evoked potential (MEP), which records muscle contraction with surface EMG attaching to peripheral muscles. In addition, EEG also has excellent temporal resolution in the scale of milliseconds. Hence, TMS-EEG expands the application of TMS in clinical research investigating cortical pathophysiology. In recent research, TMS-EEG has been implemented to assess motor and non-motor cortical functions in several diseases such as stroke, movement disorders (mainly Parkinson`s disease), dementia (predominantly Alzheimer`s disease), amyotrophic lateral sclerosis…etc. In addition, TMS-EEG also demonstrated the feasibility of investigating pharmacological or non-pharmacological treatments. Stroke patients present ‘simplified’ oscillate (less complexity) The TMS evoked potential (TEP) on the affected hemisphere in the acute stage. In the subacute and chronic stages, the alpha power in TEP increase correlated with motor recovery. The TEP in patients with Parkinson's Disease (PD) revealed decreased motor cortical excitability at the off state and reversed cortical excitability at the on state, reflecting the abnormal basal ganglia-thalamocortical activities. In addition, the DBS treatment effect could also be observed in TEP. A recent work applying TEP in patients with Alzheimer’s disease to measure some neural network activities revealed that patients with AD presented impaired default mode network by TMS targeting Precuneus, whereas the frontal-pariental network is intact when stimulating DLPFC. Furthermore, in patients with ALS, TEP demonstrated cortical disinhibition. These evidence indicates that TEP could be a potential biomarker in neurological disorders involving cortical or subcortical pathophysiology.
TMS and EEG co-registration (TMS-EEG) is a newly developed technique to record the post-synaptic potential on the cortex evoked by TMS. TMS-EEG provides more information on cortical physiology than conventional motor-evoked potential (MEP), which records muscle contraction with surface EMG attaching to peripheral muscles. In addition, EEG also has excellent temporal resolution in the scale of milliseconds. Hence, TMS-EEG expands the application of TMS in clinical research investigating cortical pathophysiology. In recent research, TMS-EEG has been implemented to assess motor and non-motor cortical functions in several diseases such as stroke, movement disorders (mainly Parkinson`s disease), dementia (predominantly Alzheimer`s disease), amyotrophic lateral sclerosis…etc. In addition, TMS-EEG also demonstrated the feasibility of investigating pharmacological or non-pharmacological treatments. Stroke patients present ‘simplified’ oscillate (less complexity) The TMS evoked potential (TEP) on the affected hemisphere in the acute stage. In the subacute and chronic stages, the alpha power in TEP increase correlated with motor recovery. The TEP in patients with Parkinson's Disease (PD) revealed decreased motor cortical excitability at the off state and reversed cortical excitability at the on state, reflecting the abnormal basal ganglia-thalamocortical activities. In addition, the DBS treatment effect could also be observed in TEP. A recent work applying TEP in patients with Alzheimer’s disease to measure some neural network activities revealed that patients with AD presented impaired default mode network by TMS targeting Precuneus, whereas the frontal-pariental network is intact when stimulating DLPFC. Furthermore, in patients with ALS, TEP demonstrated cortical disinhibition. These evidence indicates that TEP could be a potential biomarker in neurological disorders involving cortical or subcortical pathophysiology.
- Time
- Topic
- Speaker
- Moderator
- 17:00-17:30
- Diagnosis and monitoring of Psychiatric disorders using evoked potentials
- Speaker:
Ming-Hsien Hsieh
- Moderator:
Hsing-Chang Ni
- Ming-Hsien Hsieh
- MD, PhD
-
Attending Physician, Department of Psychiatry, National Taiwan University Hospital and College of Medicine, Taipei, Taiwan
E-mail:hsiehmingh@ntu.edu.tw
Executive Summary:
Dr. Ming-Hsien Hsieh accomplished his psychiatry specialist training at National Taiwan University Hospital, Taipei, Taiwan. He became the attending psychiatrist since 1999. He engaged in the research of event-related potential studies of psychiatric disorders since then, and had been to the Psychiatry Department of UCSD as a research scholar under the mentorship of Prof. David Braff and Prof. Gregory A. Light from 2003 to 2004. Currently, Dr. Hsieh is the ERP-Lab director in Department of Psychiatry, National Taiwan University Hospital.
Dr. Hsieh’s major research fields are auditory event-related potentials: P50, MMN (mismatch negativity) and Gamma ASSR in patients with psychiatric disorders. How these preattentional, automatic information processing ERPs are differentiated and the relationship between ERPs with genes, neuroimaging, and neurocognition is essential to psychiatrists. Besides schizophrenia, the ERP-Lab also recruits subjects with other psychiatric disorders, for example, suspected pre-psychotic state, autistic disorder, autism spectrum disorders, and ADHD. Additionally, novel ERP analyzing techniques have been applied, including time-frequency analysis, source localization, machine learning, etc.
Dr. Ming-Hsien Hsieh accomplished his psychiatry specialist training at National Taiwan University Hospital, Taipei, Taiwan. He became the attending psychiatrist since 1999. He engaged in the research of event-related potential studies of psychiatric disorders since then, and had been to the Psychiatry Department of UCSD as a research scholar under the mentorship of Prof. David Braff and Prof. Gregory A. Light from 2003 to 2004. Currently, Dr. Hsieh is the ERP-Lab director in Department of Psychiatry, National Taiwan University Hospital.
Dr. Hsieh’s major research fields are auditory event-related potentials: P50, MMN (mismatch negativity) and Gamma ASSR in patients with psychiatric disorders. How these preattentional, automatic information processing ERPs are differentiated and the relationship between ERPs with genes, neuroimaging, and neurocognition is essential to psychiatrists. Besides schizophrenia, the ERP-Lab also recruits subjects with other psychiatric disorders, for example, suspected pre-psychotic state, autistic disorder, autism spectrum disorders, and ADHD. Additionally, novel ERP analyzing techniques have been applied, including time-frequency analysis, source localization, machine learning, etc.
Lecture Abstract:
Clinical use of Event-related potentials in Psychiatry disorders
An evoked potential (EP) or Event-related potential (ERP) is the time-locked average of the EEG in response to a specific sensory, motor or cognitive event. Sensory evoked or ‘exogenous’ potentials are recordings of cerebral or spinal potentials elicited by stimulation of specific sensory pathways (e.g., SSEP, VEP, BAEP). In contrast, ERP depend upon the mental attention of the subject and the setting in which the stimulus occurs, rather than simply on the physical characteristics of the stimulus.
In this lecture, I will briefly discuss clinical role of event-related potential in psychiatry disorders. Take MMN (mismatch negativity) for example, it reflects the brain's automatic response to changes in auditory stimuli. It has gained attention in psychiatry as a potential biomarker for various disorders, particularly schizophrenia and psychotic disorders. Here are some detailed insights:
(1) Biomarker Potential: Reduced MMN amplitude is a robust finding in patients with chronic schizophrenia, and there are well-established animal models of MMN.
(2) Neurophysiological Insights: MMN reflects preattentive auditory sensory memory and is associated with N-methyl-D-aspartate (NMDA) receptor function, which plays a fundamental role in the pathophysiology of schizophrenia.
(3) Stability and Predictive Utility: Research indicates that MMN amplitude is relatively stable over time, making it useful for tracking illness progression. It has also been linked to worsening auditory hallucinations, everyday functioning, and illness severity in chronic psychotic disorders.
(4) Early Intervention: MMN has shown potential as a "translatable" brain marker for early intervention in psychosis. Studies suggest that individuals in the early stages of psychotic disorders exhibit attenuated MMN amplitude, which could help predict the risk of developing psychosis.
While ERPs are not yet mainstream diagnostic tools, ongoing research emphasizes their utility in supplementing traditional methods to enhance objectivity and personalization in psychiatric care.
Clinical use of Event-related potentials in Psychiatry disorders
An evoked potential (EP) or Event-related potential (ERP) is the time-locked average of the EEG in response to a specific sensory, motor or cognitive event. Sensory evoked or ‘exogenous’ potentials are recordings of cerebral or spinal potentials elicited by stimulation of specific sensory pathways (e.g., SSEP, VEP, BAEP). In contrast, ERP depend upon the mental attention of the subject and the setting in which the stimulus occurs, rather than simply on the physical characteristics of the stimulus.
In this lecture, I will briefly discuss clinical role of event-related potential in psychiatry disorders. Take MMN (mismatch negativity) for example, it reflects the brain's automatic response to changes in auditory stimuli. It has gained attention in psychiatry as a potential biomarker for various disorders, particularly schizophrenia and psychotic disorders. Here are some detailed insights:
(1) Biomarker Potential: Reduced MMN amplitude is a robust finding in patients with chronic schizophrenia, and there are well-established animal models of MMN.
(2) Neurophysiological Insights: MMN reflects preattentive auditory sensory memory and is associated with N-methyl-D-aspartate (NMDA) receptor function, which plays a fundamental role in the pathophysiology of schizophrenia.
(3) Stability and Predictive Utility: Research indicates that MMN amplitude is relatively stable over time, making it useful for tracking illness progression. It has also been linked to worsening auditory hallucinations, everyday functioning, and illness severity in chronic psychotic disorders.
(4) Early Intervention: MMN has shown potential as a "translatable" brain marker for early intervention in psychosis. Studies suggest that individuals in the early stages of psychotic disorders exhibit attenuated MMN amplitude, which could help predict the risk of developing psychosis.
While ERPs are not yet mainstream diagnostic tools, ongoing research emphasizes their utility in supplementing traditional methods to enhance objectivity and personalization in psychiatric care.